We use cookies to make your experience better. To comply with the new e-Privacy directive, we need to ask for your consent to set the cookies. Learn more.
What is Endometriosis?
March is international Endometriosis Awareness Month. Around 1 in 10 people who menstruate are diagnosed with endometriosis: that’s approximately 200 million people.
And yet, it takes an average of 7 years to get diagnosed, and—even more surprisingly—there’s still no cure.
Incidentally, that’s how long my diagnosis took. I asked countless doctors for help. My symptoms got so bad that I was afraid to leave my house even if I felt ok. At any moment, I could become completely debilitated—vomiting, unable to walk and losing my vision from the pain.
I quickly realised that there is a constant denial that our pain is anything other than “normal period pain”.
One of the many miserable results of sex discrimination is the stigma surrounding periods. We’re afraid to talk about it! It’s messy and raw and confronting. Half the population bleeds out their vagina every month, and yet, we barely teach our children how to talk about it.
We’re told to just accept that people who menstruate must learn to live with the side effects—even when those side effects might actually be signs of a real problem. And to make matters worse, once you finally find someone who believes your pain is real, you then have to go through the notoriously difficult diagnosis process.
No wonder it takes so long to get help!
I dream that one day, our children will be able to ask for help and know that someone is listening. We need endometriosis awareness so that people who menstruate don’t continue to live in a world where their pain is denied.
So, what is endometriosis?
Endometriosis is a progressive, chronic disease.
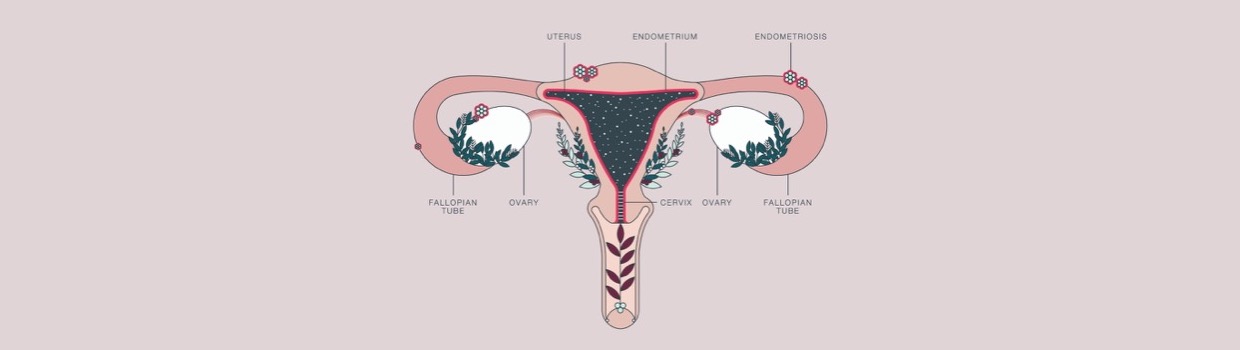
First, it is important to know what the endometrium does. Simply put, the endometrium is a lining of the uterus.
Each month, at the beginning of the menstrual cycle, oestrogen helps the endometrium thicken in preparation for an embryo (a fertilised egg). After ovulation, the body releases progesterone, which helps the endometrium secrete the fluids needed for developing an embryo. These fluids also keep the structure of the endometrium intact.
If an embryo implants itself, a pregnancy hormone will support the uterus. If an embryo doesn’t implant, then progesterone levels will decrease, and the endometrium will stop releasing the fluids and blood that hold it together. The endometrium will then break down and be released from the uterus, out through the vagina.
This is what we call a period!
Once the endometrium has been shed, the cycle starts all over again.
Endometriosis occurs when endometrium-like tissue grows outside the uterus in other parts of the body. It is mainly found on the ovaries, fallopian tubes and tissue around the pelvis. But it can also spread to any other organ in the body.
This tissue responds to menstrual cycle hormones, causing it to thicken, break down and bleed, just like the endometrium. When this happens, the tissue can’t exit the body, and it gets trapped inside. This can lead to cysts on the ovaries (endometriomas), scar tissue, inflammation and adhesions (tissue that causes the organs to stick to each other).
Types of Endometriosis
Endometriosis is classified into 4 stages:
- Minimal/Stage I
A few growths on the surface of the tissue
- Mild/Stage II
More than a few growths that extend deeper into the tissue
- Moderate/Stage III
A high number of deep growths
Small cysts on the ovaries
Adhesions occurring around the organs
- Severe/Stage IV
A high number of deep growths
Large cysts on the ovaries
Many dense adhesions affecting the organs
Pain is the most common symptom of endometriosis. However, the level of pain does not necessarily indicate the severity of the disease. People with mild endometriosis might experience severe pain, while those with extensive endometriosis might not feel any pain at all.
What causes endometriosis?
Although endometriosis is the second most common gynaecological condition, no one quite knows what causes it. The complexity of the disease suggests a combination of factors might be at play.
Some theories about the causes of endometriosis include:
- Retrograde menstruation
This theory proposes that blood and tissue from the uterus travel backwards, through the fallopian tubes and into the abdomen during menstruation. The cells then stick to the organs and begin to grow. However, nearly all people who menstruate experience retrograde menstruation and the links between retrograde menstruation and endometriosis are weak.
- Coelomic metaplasia
The cells outside the uterus may mutate and turn into endometrium-like cells. This could be triggered by hormones or immune factors. This theory would help explain the occurrence of endometriosis in strange places, like fingers or legs.
- Endometrial cell transport
Endometrial cells might travel from the uterus through the blood vessels or lymphatic system to reach other organs in the body.
- During surgery
Endometrial cells may be spread during surgery (e.g., C-section or hysterectomy).
- Genetics
Research has shown that endometriosis is 7 to 10 times more common when a close relative also has the disease.
- Immune system disorder
If retrograde menstruation occurs, the immune system might not be able to recognise or destroy endometrial-like tissue when it’s growing outside the uterus. Research has shown that immune system disorders and some types of cancer are more prevalent in women with endometriosis.
Symptoms of endometriosis
The symptoms of endometriosis can vary greatly between cases. Some people might not experience any symptoms at all, while others may find the disease extremely debilitating. Endometriosis is a progressive disease, which means the symptoms can become worse over time. For some people, certain symptoms may be constant, and for others, they may be cyclical.
The common signs and symptoms of endometriosis include:
- Pain
- Painful periods that restrict you from going about your everyday life
- Pain during or after sex
- Pain during bowel movements or weeing
- Painful ovulation, including pain in the thigh or leg
- Lower back and abdominal pain
- Irregular or very heavy bleeding or bleeding between periods
- Infertility
- Fatigue
- Irregular bowel movements, including diarrhoea and constipation
- Bleeding from the bladder or bowel
- Needing to urinate frequently
- Abdominal bloating
- Nausea
- Migraines and/or headaches
- Anxiety and depression due to chronic pain.
How is endometriosis diagnosed?
Diagnosing endometriosis is difficult and often takes around 7 to 10 years. The typical stages of diagnosis include:
1. History and physical examination
Minimal/mild endometriosis can’t be felt during a physical examination. However, if a person has moderate/severe endo, a doctor may be able to feel cysts during a gynaecological assessment.
2. Imaging
a) Ultrasound
Minimal/mild endometriosis can’t be seen using an ultrasound. But moderate/severe endometriosis may be visible if the ultrasound is performed by a specially trained person.
b) MRI
MRIs can’t show minimal/mild endometriosis but can reveal the extent of moderate/severe endometriosis.
3. Laparoscopic surgery
Surgery is the only sure way to diagnose endometriosis.
Keyhole surgery is performed using a tiny camera inserted into the abdomen to look for endometriosis growths. If growths are found, then samples are taken and sent to pathology. This is called a biopsy and will confirm whether the cells are endometrial-like.
During surgery, the doctor may remove any growths. This can be done by abrasion (burning the growths off) or excision (cutting the growths out). Excision is the most effective means of removing the growths and is the recommended procedure.
Sometimes, a doctor might prescribe hormonal medicines without a definitive diagnosis. If the treatment helps with the symptoms, then surgery may not be needed.
How is endometriosis treated?
There is no cure for endometriosis. However, the symptoms can be managed to increase your ability to enjoy life. This often includes a mixture of medical treatments and lifestyle changes.
Living with endometriosis can be extremely challenging, and seeking diagnosis and treatment is often a long, frustrating process. I recommend joining support groups and talking to other people experiencing endometriosis. When I was first diagnosed, I joined 3 online support groups and started monthly sessions with a clinical psychologist. Looking after your mental health while living with endometriosis will drastically improve your wellbeing and ability to manage your symptoms.
- Pain killers
Pain can be treated using over the counter medicine, such as ibuprofen or naproxen. However, these are not always effective.
- Natural therapy
Alternative medicine may help with the pain and other associated symptoms of endometriosis. This might include acupuncture, chiropractic care, pelvic floor physio or herbs and supplements. Dietary and lifestyle changes will often lead to positive results. A dietician or naturopath can help you figure out what changes are going to help you the most.
- Hormonal contraceptives
Birth control pills, patches, IUDs, vaginal rings and Depo-Provera injections may be used to reduce pain. By controlling your hormones and only having a period every 3 months (or not at all), the endometrium will not develop each month, and the endometrial growths will slow down. However, there are many potential side effects to consider before opting to use hormonal contraceptives. Other hormonal treatments include:
- Gonadotropin-releasing hormone (GnRH) agonist and antagonists
These block the production of oestrogen, preventing menstruation and creating artificial menopause. This treatment can cause side effects, such as hot flashes and vaginal dryness.
- Danazol
This stops menstruation and reduces symptoms. Endometriosis may continue to develop, and the drug causes side effects such as acne and increased hair growth.
- Surgery
This might involve conservative laparoscopic surgery to remove endometrial growths without damaging the reproductive organs (see above, ‘How is endometriosis diagnosed’).
As a last resort, a hysterectomy might be performed (removing the uterus, cervix and ovaries). Hysterectomy is not a cure for endometriosis. Pregnancy is not possible after a hysterectomy, and early-onset menopause will occur. However, for some people with severe endometriosis, it can improve their symptoms.
Find more information about endometriosis
The following organisations provide helpful information about endometriosis:
Endometriosis.org provides a worldwide list of support groups. There are also many online support groups where you can discuss your experiences with other endo-survivors (e.g., through Facebook or other social media sites).
This article is intended for general purposes only. If you think you might have endometriosis, please consult your medical practitioner for further advice.
Written by Nina Giblinwright
Image by Duvet Days
